Patellofemoral pain syndrome (PFPS) is describing the front knee pain around the patella or kneecap. We also call it “runner’s knee” or “jumper’s knee” because it’s more common in those who take part in sports that involve running and jumping significantly females and young adults. Patellofemoral pain syndrome is usually caused by imbalances within the muscles encompassing the knee joint, which influences the kneecap and cartilage within the joint. However, patellofemoral pain syndrome will occur in normal individuals.
The pain and stiffness will make it troublesome to climb stairs, kneel down, and perform other daily activities.
Many things might contribute to the development of patellofemoral pain syndrome. Problems with the alignment of the kneecap and overuse from vigorous athletics or training are usually important factors. Knee pain typically will increase when you run, walk up or down stairs, sit for long periods, or squat.
The differential diagnosis of PFPS includes chondromalacia patella and patellar tendinopathy. We don’t think about both underneath the umbrella term of PFPS, though patients can complain of similar symptoms. The pathophysiology is different and so there needs accurate treatment.
Patellofemoral pain usually relieves with conservative treatment, like rest and ice and changes in activity levels or sometimes needs physiotherapy to set therapeutic patellofemoral pain syndrome exercises to ease the pain.
Patellofemoral Pain Syndrome vs Chondromalacia Patella
Chondromalacia patella is one of the most frequent causes of chronic knee pain. Chondromalacia patella proceeds from the degeneration of cartilage because of poor alignment of the kneecap as it slides over the lower end of the thighbone/femur. It sometimes refers to this process as patellofemoral syndrome.
Anatomy
The healthy knee joint comprises bones, cartilage, ligaments, and tendons. The knee joint is the largest joint in our body and one among the most complex joints. It comprises the lower end of the femur, the upper end of the tibia, and therefore the patella. The knee comprises two major joints, the tibiofemoral joint and therefore the patellofemoral joint.
Ligaments and tendons connect the femur to the tibia. The four major ligaments attach to the bones and act like robust ropes to carry the bones together. Muscles are connected to bones by tendons. The quadriceps tendon connects the muscles within the thigh’s front to the patella.
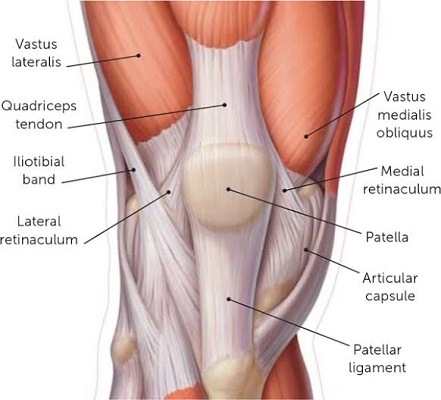
The patella sits within the femoral groove; The facies articularis patella (posterior side) is covered with cartilage that glides over the cartilage of the anterior part of the femoral condyles. During this synovial joint movement and gliding creates marginal resistance because of the synovial fluid present around the knee and produced by the synovial membrane, the inner part of the joint capsule during movement. The articular cartilage helps our bones glide smoothly against one another as you move your leg.
Although every ligament has its responsibility in supporting and protecting the knee, ligaments conjointly give assistive support to other ligaments. However, the two ligaments that are most related to PFPS are the lateral and medial collateral ligaments, because they are incorporated with the knee capsule. Epicondylopatellar and meniscopattelar ligaments form the medial and lateral retinaculum patellar a part of a ligamentous complex that provides for a medial and lateral attachment of the patellar tendon at the level of the patella.
Also aiding in movement is the synovium—a skinny lining of tissue that covers the surface of the joint. The membrane produces a small amount of fluid that lubricates the cartilage. Also, just under the kneecap is a tiny pad of fat that cushions the kneecap and acts as a shock absorber.
Patellofemoral Pain Syndrome Symptoms
The most typical symptom of patellofemoral pain syndrome is a dull, aching pain within the knee’s front. This pain typically begins bit by bit and is usually activity related which will be present in one or both knees. Patellofemoral pain symptoms are usually seen during weight-bearing or jarring activities that involve knee bending. Other typical symptoms encompass:
- Exercise and activities induce pain that repeatedly bends the knee, like walk-up/ climbing stairs or downstairs, running, jumping, or squatting.
- Pain after sitting for an extended period along with your knees bent.
- The pain throughout or after you have played sport.
- Popping or crepitation sounds in your knee once climbing stairs or once standing up after prolonged sitting.
The symptoms of patellofemoral pain will vary from time to time. As your patellofemoral pain syndrome advances, your knee can become painful while walking and then finally even at rest.
Patellofemoral Pain Syndrome Causes
Patellofemoral pain syndrome is usually caused by patellar trauma; however, it is more often a combination of many factors: overuse and overload of the patellofemoral joint, anatomical or biomechanical abnormalities, muscular weakness, imbalance, or dysfunction.
One of the most common causes of PFPS is patellar orientation and alignment. Once the patella encompasses a different orientation, it will glide more to one side of the facies patellar (femur) and so will cause overuse/overload on it a part of the femur which might cause pain, discomfort or irritation. Different causes will provoke such deviations.
The patellar orientation varies from one patient to another; It may also differ from the left to the correct knee within the same individual and may result from anatomical mal-alignments. A bit of deviation of the patella will cause muscular imbalances, biomechanical abnormalities, which may cause PFPS. Conversely, muscular imbalances or biomechanical abnormalities cause a patellar deviation and conjointly provoke PFPS. For example: once the Vastus Medialis Obliquus isn’t sufficiently strong, the Vastus Lateralis will bring to bear a higher force and may produce a lateral glide, lateral tilt or lateral rotation of the patella which may cause an overuse of the lateral aspect of the patellar and lead to pain or discomfort. Another muscle and ligament which will cause a patellar deviation is an iliotibial band or the lateral retinaculum just in case there’s an imbalance or weakness in one of these structures.
PFPS may also be because of knee hyperextension, lateral tibial torsion, genu valgum or varus, increased Q-angle, tightness within the iliotibial band, hamstrings or gastrocnemius.
Repeated trauma causes an increase in your retro patellar joint forces, which may cause kneecap pain, joint irritation, and eventually degeneration of your patella joint surface.
Patellofemoral pain affects 25% of the population in their lives; however, it is more common in athletes. Sports, where patellofemoral pain syndrome is usually seen in running, jumping and landing, or squatting position, is required. Sports embody running, tennis, netball, football, volleyball, basketball, skiing and different jumping sports.
Patellofemoral pain syndrome is additionally common during adolescence as a result of the long bones developing quicker than the muscles, tendons, and ligaments, putting unexpected stresses on the joints. It predisposes active youngsters who don’t stretch to patellar mal-alignment.
Poor foot posture and weak hip control muscles will both permit your knee to abnormally twist and lead to a lateral deviation of your patella. The poor biomechanics of walking or running patterns can induce patellofemoral pain.
At a glance Patellofemoral Pain Syndrome
- Running or jumping sports puts repetitive stress on the knee joint, which may irritate the kneecap.
- Patellofemoral pain will occur once the muscles around your hip and knee do not keep your kneecap properly aligned. It associates inward movement of the knee during a squat that induces patellofemoral pain.
- Biomechanical problems will cause Patellofemoral Pain Syndrome.
- It has linked trauma to patellofemoral pain syndrome.
- Knee surgery particularly repairs to the anterior cruciate ligament using your patellar tendon as a graft, will increase the chance of patellofemoral pain.
Untreated patellofemoral pain syndrome may also predispose you to patellar tendonitis.
You May Like:
- Best Shoes For Plantar Fasciitis As Per User Reviews
- Most Comfortable Steel Toe Boots For Standing All Day
Patellofemoral Pain Syndrome Diagnosis
Patellofemoral pain syndrome is fairly simple to diagnose. Your knee specialist or physical therapist can make a diagnosis based on symptoms and physical examination of the knee. During the physical examination, your doctor can discuss your general health and therefore the symptoms you are experiencing. Your doctor will ask when your knee pain started and the severity of the pain. Your physician will ask you what activities cause the pain to worsen.
To check for any changes behind your kneecap that might cause your symptoms, your doctor could ask you to tighten your quadriceps muscles whereas they hold your kneecap down, as this can reproduce the pain.
During the examination, your doctor can check your knee for problems in patellar tracking. to see the precise location of the pain, your doctor could gently press and pull on the front of your knees and kneecaps. He or she can also ask you to squat, jump, or lunge during the examination to check your knee and core body strength.
Occasionally, the increased fluid within the joint will cause swelling; Thus, your knee specialist or physical therapist will check for this.
To help diagnose the reason behind your pain and to rule out the other physical issues, your physician can also check:
- Alignment of the lower leg and the position of the kneecap
- Check knee stability, hip rotation, and the range of motion of the knees and hips
- The kneecap for signs of tenderness
- The attachment of thigh muscles to the kneecap
- Strength, flexibility, firmness, and tone of the hips, front thigh muscles (quadriceps), and back thigh muscles (hamstrings)
- The tightness of the heel cord and flexibility of the feet
Finally, your doctor might ask you to walk back and forth to look at your gait. He or she will search for issues along with your gait that will contribute to your knee pain.
Blood tests don’t help in the identification of patellofemoral pain syndrome; However, it is also helpful for ruling out more serious issues. Usually, your doctor can diagnose patellofemoral pain syndrome with a physical examination. X-rays aren’t typically useful as cartilage doesn’t show up on them. Your doctor could recommend a magnetic resonance imaging (MRI) scan, as an example, if you’ve had a blow to your knee.
Patellofemoral Pain Syndrome Treatment
Management of patellofemoral pain syndrome often begins with simple steps. Rest your knee as much as possible. Avoid or change activities that enhance the pain, such as kneeling, climbing stairs, or squatting.
Home Remedies for Patellofemoral Pain Syndrome
Most times, patellofemoral pain will improve with simple home treatment. The RICE protocol is used for an acute stage. Stop doing the activities that make your knee hurt until your pain resolves. This may imply change your training routine or swapping to low-impact activities that will put less stress on your knee joint. Biking and swimming are good low-impact options. If you are obese, losing weight will further help to diminish pressure on your knee.
Medication for Patellofemoral Pain Syndrome
Simple painkillers (analgesics) such as paracetamol can help to ease the pain. Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can help reduce swelling and relieve pain. Non-steroidal anti-inflammatory drugs (NSAIDs) may not offer any additional benefit over paracetamol, and NSAIDs are more likely to have side effects.
If your pain persists, or it becomes more difficult to move your knee, contact your knee specialist or physical therapist for a thorough evaluation.
Your doctor design medical treatment for patellofemoral pain syndrome to relieve pain and restore range of motion and strength. In most cases, patellofemoral pain can be treated nonsurgically.
Nonsurgical Treatment for Patellofemoral Pain Syndrome
Besides activity changes, the RICE method, anti-inflammatory drug, and your doctor may recommend:
Physiotherapy for Patellofemoral Pain Syndrome
It’s crucial to keep your quadriceps strong and balanced to escape putting pressure on your knee joint. Your doctor may give you exercises to do or suggest that you see a physiotherapist who will suggest other exercises. They’ll evaluate your knee and decide what’s making your pain and which exercises regime will best fit for your particular problem. They’ll also make sure you’re doing the exercises properly and safely.
It may take at least 12 weeks of doing exercises several times a day for 30 minutes a day before any muscle imbalance or weakness is corrected, and it could be after that until the pain completely settles down.
Lists of common interventions to treat PFPS below:
- Manual Therapy
- Exercises
- Quadriceps strengthening
- Patellar Taping
- Knee Braces
- Proximal muscle strengthening
- Electrotherapy Modalities
Patellofemoral Pain Syndrome Exercises
It’s essential to exercise your thigh muscles to stop them from becoming unstable. Swimming is an excellent form of exercise, and the front and back crawl will put less strain on your knees. You should escape sports that put extra pressure on your knees, like rugby, football, or running, if it makes the pain worse, you will start this once the symptoms have eased.
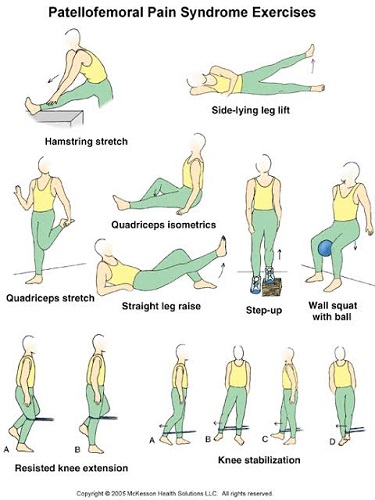
Wall Squats are Helpful if You do it Regularly-
- You will stand with your back against a wall and feet together.
- Then you will slide down the wall by bending your knees until you will no longer look at your toes.
- Now you will hold this position for 8–10 seconds.
- Repeat the exercise 8 times and complete 3 sets.
Your Physiotherapist May Recommend Additional Exercises-
Specific exercises for patellofemoral pain will help you improve your range of motion, strength, and endurance. It is especially important to focus on strengthening and stretching your quadriceps since these muscles are the main stabilizers of your kneecap. It may also recommend core exercises to strengthen the muscles in your abdomen and lower back.
Proprioceptive Training
It has been proven that improving proprioceptive quality in the knee of patients that will reduce patellofemoral pain. Even with unilateral PFPS, it decreases proprioception in both knees. Therefore, proprioceptive training (pain-free exercises) of the knee should be part of the rehabilitation program.
Electrotherapy
Some patients might suffer from PFPS because of a (neuromuscular) imbalance between the VMO and VL. The main cause is muscle atrophy of the VMO and excessive/abnormal lateral tracking of the patella, because of the remaining force of the VL. With neuromuscular imbalance between the VMO and VL, it should consider electrical stimulation of the VMO to complement the conservative (exercises) therapy, because it is selective and does not stress the patellofemoral joint. It may use the TENS machine or EMS as one part of a patellofemoral pain syndrome management program or muscle rehabilitation under the guidance of your physical therapist.
If you play sport and depending on the demands of your chosen sport, you may require specific sport-specific exercises, and a progressed training regime to enable a safe and injury-free return to your chosen sport. Your physiotherapist will discuss your goals, timeframes, and training schedules with you to optimize you for a complete and safe return to sport. The perfect outcome will have you performing at full speed, power, agility, and function thorough rehabilitation program has minimized your chance of future injury.
Patellofemoral Pain Syndrome Braces
Knee braces can further prevent or diminish the symptoms of Runner’s Knee and patellofemoral pain syndrome. Runner’s knee usually occurs because of muscle imbalance, overuse, mal-alignment and more.


Shoe Inserts for Patellofemoral Pain Syndrome
Stretching likewise diminishes the uneven pull of the muscles. If foot biomechanics lead to your knee pain, insoles or orthotics with strong arch support will support you. The shoe inserts prevent the inward rotation of the knee that results from the overpronation of the foot.


Shoe inserts can help align and stabilize your foot and ankle, taking the stress off of your lower leg. Orthotics can either be custom made for your foot or purchased “off the shelf.” Shoe inserts take the stress off your lower leg by aligning your foot and ankle.
Patellofemoral Pain Syndrome Taping

Taping can lessen pain in the knee. There are various methods of taping, but the common enforcer is to exert a medially directed force on the patella to enhance the patellofemoral contact area, decreasing joint stress and reducing pain.
Surgical Treatment for Patellofemoral Pain Syndrome
Patellofemoral pain syndrome is rarely needed surgery and is done only for severe cases that do not respond to nonsurgical treatment. Surgical treatments may include:
Arthroscopy
During arthroscopy, your physician will insert a small camera, called an arthroscope, within your knee joint. The camera exposes pictures on a television screen, and your surgeon uses these pictures to guide miniature surgical devices.
- Debridement– Sometimes, removing damaged articular cartilage from the surface of the patella can provide pain relief.
- Lateral release– If your lateral retinaculum tendon is stiff enough to pick the patella out of the trochlear groove, a lateral release operation can loosen the tissue and revise the patellar malalignment.
If tightness in the lateral retinaculum is pulling your kneecap to the side, your doctor may recommend lateral release surgery to cut the ligament.
Tibial Tubercle Transfer
Sometimes, it may be significant to realign the kneecap by turning the patellar tendon along with a segment of the tibial tubercle—the bony prominence on the shinbone.
It requires a traditional open surgical incision for this procedure. The surgeon partially or totally separates the tibial tubercle so that the bone and the tendon can be moved toward the medial side of the knee. The piece of bone then reattached to the tibia by using screws. In most instances, this transfer provides better tracking of the kneecap within the trochlear groove.
Patellofemoral Pain Syndrome Prevention
Leg extension exercises help to strengthen and stretch the quadriceps, the muscles in the thigh’s front. It is essential to strengthen, stretch, and maintain accurate conditioning of the muscles around the knee, particularly the quadriceps and the hamstrings. If you’re overweight, losing weight relieves stress on your knees.
Patellofemoral pain syndrome is generally perfectly relieved with simple measures and with physical therapy. It may persist if you do not make modifications to your training program or activity level. Make sure your shoes fit well and produce good shock absorption. If you have flat feet, think about shoe inserts.